As omicron becomes the latest COVID-19 twist to upend schools’ plans, several K-12 leaders shared in a virtual panel Tuesday four ways their COVID-19 testing programs successfully function: having a district testing champion, supporting school nurses, partnering with community resources and standardizing communication with families.
These leaders spoke at The Rockefeller Foundation’s Learning Network’s final virtual panel after a series of weekly meetings to review best approaches for effectively implementing COVID-19 testing in schools. The panel was held as the omicron variant spreads and becomes the dominant COVID-19 strain in the U.S.
The foundation is working to create a national COVID-19 testing program in K-12 schools and has spent the past two months collaborating with about 30,000 schools in its Learning Network across 26 states and Washington, D.C.
After the Centers for Disease Control and Prevention announced guidelines for K-12 test-to-stay programs Friday, President Joe Biden said in a Tuesday address to the nation that this CDC guidance will help schools stay open even if a student tests positive.
Test-to-stay policies have gained traction among districts in recent months, but experts suggest the testing strategy is only effective on top of other mitigation measures, including masking, social distancing and vaccination.
Testing strategies can vary by district. Some schools only test unvaccinated students while others test all students from willing families. Testing measures can range from PCR pooled testing to rapid antigen testing, as well.
No matter the exact approach, the virtual Learning Network panel offered four takeaways for district leaders to consider as they develop or work to improve their own K-12 testing programs.
Have a COVID testing champion
It’s important to combat misinformation and political tension with knowledge if controversy over K-12 COVID-19 testing emerges during school board meetings, said Brittany Layman, health and wellness coordinator at Regional School Unit 22 in Hampden, Maine.
“To make this program run, you need to have a really strong and clear understanding of how it works — everything from the consent process to the testing process, where those samples go and how information is kept private,” Layman said.
Districts also need a “testing champion,” Layman said, specifically a superintendent and principal who can cheer on testing practices and articulate and answer any questions that may surface during public school board meetings.
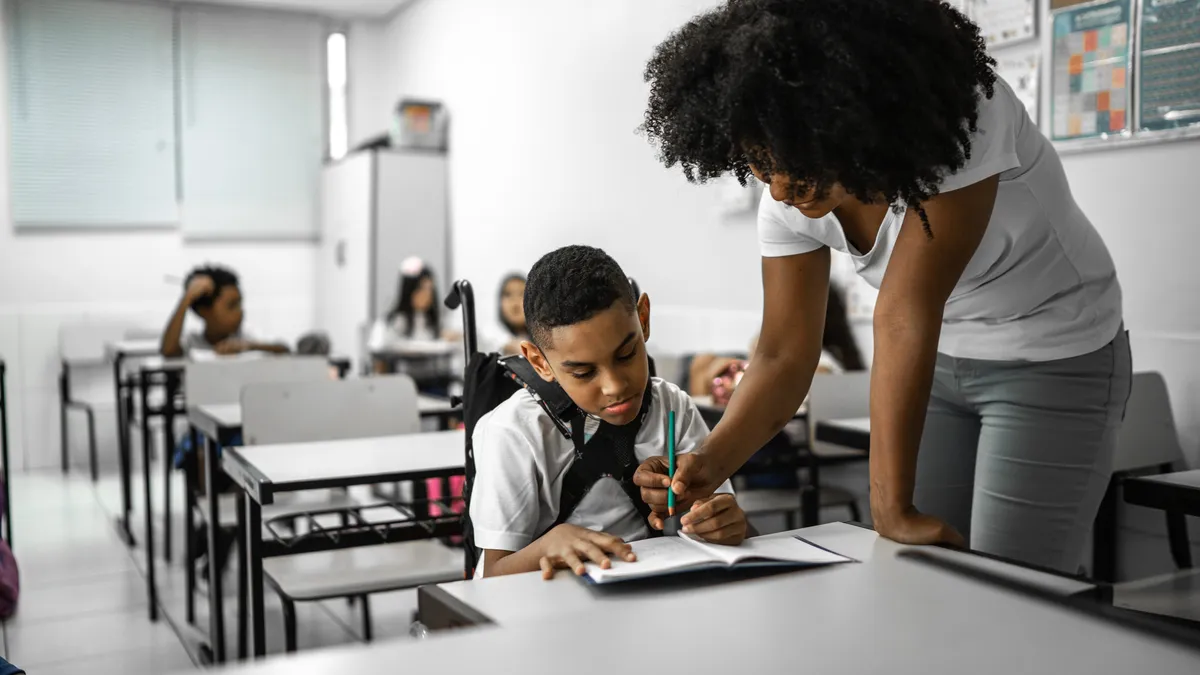
Support school nurses
With the ongoing nationwide nurse shortage, it was key for Kisha Borden, president of the San Diego Education Association, to negotiate with the San Diego Unified School District’s school board on how to recruit school nurses. Sure enough, the union was able to secure a $4,000 hiring incentive per school nurse in collaboration with district leadership, Borden said.
“As we returned to school this fall, we saw that as the only medical professionals on the school site, a lot was being put on the plates of our school nurses,” Borden said. “We heard from our nurses that they were really overwhelmed, stretched to their breaking point.”
That led the union to also urge the school board to hire an outside vendor to complete contact tracing and help ease the burden on school nurses, she said.
At Mastery Charter Schools in Philadelphia and Camden, New Jersey, the school system also began developing a strategy early on to minimize the need for additional school nursing staff, said Laura Clancy, Mastery Charter Schools’ health and safety chief.
Specifically, the school system was able to hire temporary non-nursing staff members to assist with everything in the testing process except sample collection, Clancy said. Then, the schools used nursing agencies to hire staff for sample collection.
Partner with community resources
Tulsa Public Schools in Oklahoma addressed its nurse shortage and high turnover by working with a local university nursing program, said Jennifer Harper, a coordinator between the district and the local health department.
The university has struggled throughout the pandemic to find work sites that would provide practicum hours or internship opportunities for nursing students, Harper said.
“We were able to step into that gap,” Harper said.
In fact, the district was able to offer practicum hours in exchange for the university nursing students' help with administering COVID-19 tests in schools. Another benefit of this relationship is that it established a pipeline for potential new school nurses, Harper said.
A key to developing this mutual relationship is to also create a standard Memorandum of Understanding agreement that defines the role of nursing students, as well as the number of practicum hours they will receive, she said.
Overall, it’s important to seek partnerships with community resources, such as pharmacies and community health centers, when possible, said Eva Stone, health manager of Jefferson County Public Schools in Louisville, Kentucky.
Streamline communication
At JCPS, Stone worked with the communications department to repurpose the district’s emergency text system to standardize messages informing students and families about COVID testing, exposures and quarantining.
One benefit is this messaging system can send texts in a family’s first language, Stone said. The system further helps nurses focus on other responsibilities instead of personally contacting families about student exposures to COVID-19. The district held a news conference to help get the word out to families about the new COVID-19 text messaging platform.
For district leaders looking to implement a similar program, Stone said, it’s key to have a good messaging system for contacting families. It’s also important to make sure to communicate with staff and provide training at the onset and to inform families that the change is coming, she said.
The Clark County School District in Nevada established a parent call center line that hired 50 registered nurses and licensed practical nurses to do contact tracing and maintain consistent messaging to families and school administrators, said Sheri McPartlin, the district’s chief nurse and student health services director.
“It’s allowed us as a district to train a smaller number of nurses whose sole focus was just COVID-19 and contact tracing, and it also allowed parents to speak to a nurse and answer questions,” McPartlin said. “So that essentially took the burden off of our school sites and our school nurses providing just direct care to students.