Four years ago Sullivan High School, a Chicago Public School on the city’s north side, was losing students. Enrollment was in decline and attendance was steadily pretty poor. The graduation rate was barely 50%.
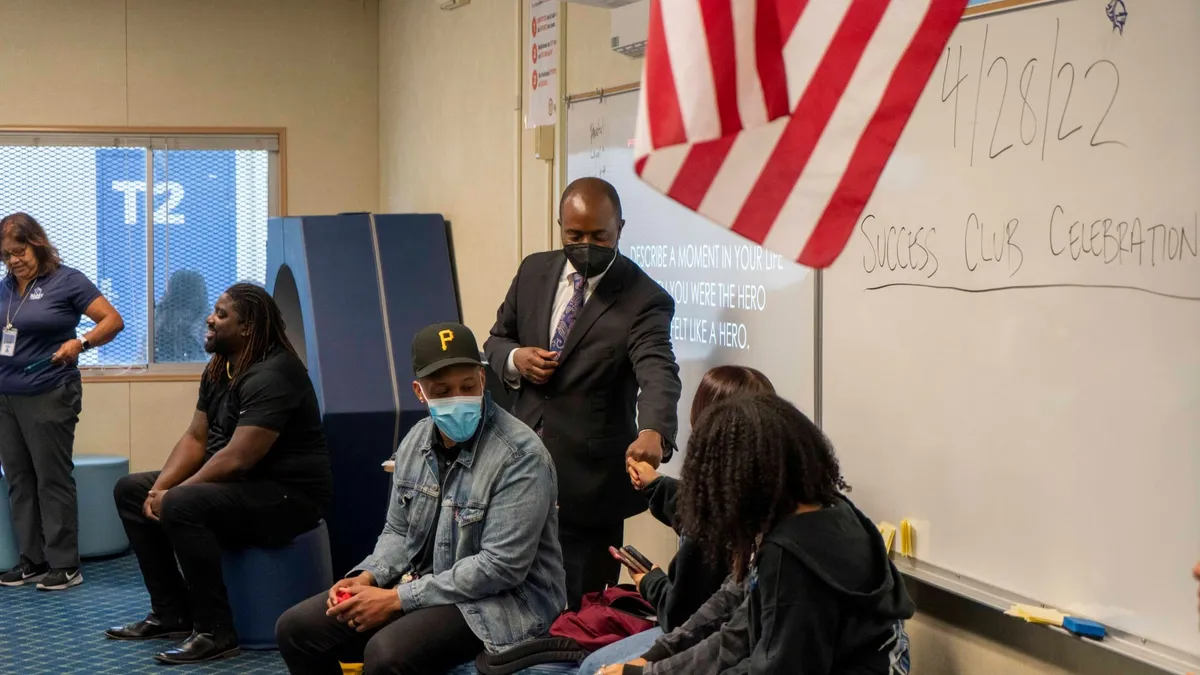
Chad Adams, who is wrapping up his fourth year as principal of Sullivan High School, points to the SMART clinic as a major contributor to very impressive gains on each of these measures. The clinic opened in 2013 with ambitious goals to proactively serve all students and, in turn, have a positive impact on academic outcomes. The prior clinic that it replaced served about 15-20% of Sullivan students. By its third year, the SMART clinic had gotten consent to serve 92% of Sullivan students and had served 92% of that subset, and even within its first year, the clinic was already seeing the majority of the student body.
Adams can see a direct correlation between these service patterns and school performance. By the second year of the clinic’s operation, average daily attendance shot up from 80% to almost 90%. Adams said the graduation rate is expected to hit 80% this year. And he said the portion of freshman on track to graduate, a measure followed closely by Chicago Public Schools, was 95% earlier this year, indicating the graduation rate should keep rising.
While the clinic isn’t the only thing happening at Sullivan, Adams says it has made a difference.
“When kids and families feel like they’re being taken care of and cared about, they start showing up more, they have more pride,” Adams said.
And word is getting around. While families had steadily been choosing charters over Sullivan before Adams started, the trend seems to have shifted. Since he has been principal, he has watched the freshman class go from 97 students to about 220.
The SMART Student Health and Wellness approach was developed by Melanie Ginn, of Ginn Group Consulting, and born out of a partnership with CVS Health Workforce Initiatives. Heartland Health Centers is the current medical provider and CVS Health continues to fund the clinic, but the model was specifically developed to be sustainable, rather than reliant on grant funding.
While the nation’s healthcare funding system continues to be in flux, the SMART clinic has found a way to do more while reducing costs. The clinic increased productivity by serving far more students, it cut overhead by using a flexible staffing model that worked around the school schedule and it dramatically increased reimbursement revenue, according to a white paper presented to members of Congress in May by Liza Cariaga-Lo, Brown University’s vice president for academic development, diversity and inclusion.
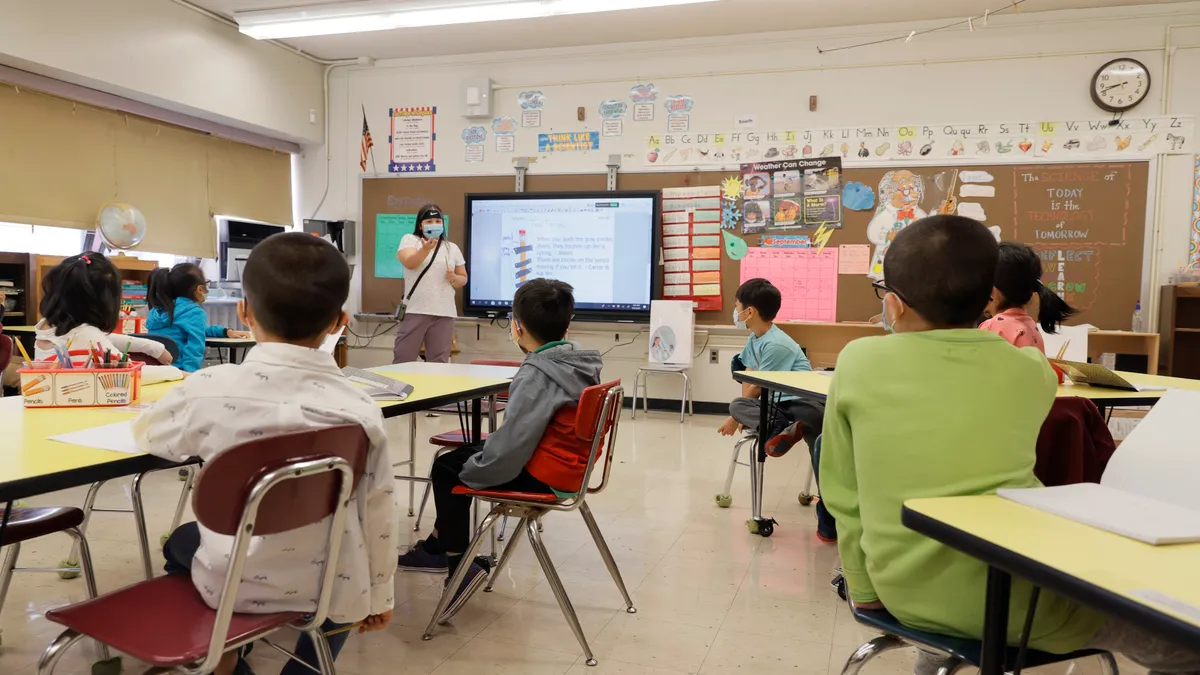
Operationally, a nurse practitioner, nurse, nurse’s assistant, doctor, social worker and receptionist serve students in an independent, but fully embedded, clinic that has become closely intertwined with the school administration. Students get pulled out of lunch and electives for appointments, and their relationship to the clinic starts with a behavior assessment and medical history. Students are pre-screened for trauma and sexual activity, and the medical staff works collaboratively to develop short-, mid-range, and long-term health goals for each student, all with an emphasis on ultimately improving academic performance. In this way, the clinic’s goals are very much in line with the school’s goals.
It hasn’t been hard for educators to see the impact of this focus. Adams said some of the work the clinic does keeps certain problems off his plate.
“If they are servicing kids and [the kids are] feeling like their needs are getting met, they’re not acting out in class as much,” Adams said, explaining that students tend to act out, do drugs or skip school in an attempt to indicate they need help. “It seems each year we’ve had less and less of that because they are getting their needs met in the clinic.”
Cariaga-Lo, in her report, highlighted the culture shift prompted by the clinic and the “stunning and swift de-stigmatization” of seeking and receiving both physical and behavioral healthcare.
“When over 90% of the students are receiving any number of types of care, wellness becomes an expectation and self-advocacy and receipt of care is normalized,” Cariaga-Lo wrote.
And prevention as well as early identification of health-related issues, both mental and physical, has long-term payoffs. Ginn Group Consulting tallied the financial impact of reproductive health counseling and contraception: $109,025 saved in healthcare costs with reproductive health counseling, $37,363 saved in preventing measles with vaccines, $41,880 saved by avoiding incarceration, and $1.2 billion added to the economy by reduced crime and increased earning stemming from a 5% increase in male high school graduates.
The school itself has also seen a direct increase in funding because of higher attendance and student retention.
There were about 2,300 school-based health centers spread across almost every state during the 2013-14 school year, the latest year for which there is comprehensive data available on such centers. The SMART model is new, but Sullivan High School shows the possibilities when a focus on proactive healthcare is embedded into school improvement.
And Adams has plans for even more comprehensive collaboration. Already, data from the clinic has contributed to needed programming about healthy relationships and access to screenings for sexually transmitted infections. The next step will be tailoring the academic curriculum to meet needs identified through the clinic, though Adams said that will be harder to coordinate than one-off workshops.
In the end, the commitment to healthcare at Sullivan High School comes down to serving the whole child. Students can focus on academics if their mental and physical health needs are not being met. And with the SMART clinic, Sullivan students can get that holistic support – to everyone’s benefit.