With unnerving frequency, school districts and communities are discovering elevated lead levels after undertaking tests of drinking water sources in their facilities. Recently, comprehensive re-testing in New York City public school buildings found that 83% of buildings had at least one water source with lead levels about 15 parts per billion, the U.S. Environmental Protection Agency’s standard level for when action must be taken on public water systems. For drinking water, the recommended action level rises to 20 parts per billion.
Considering the firestorm of controversy that engulfed Flint, MI, in the past several years, cities and school districts around the country are anxious about potential lead levels in drinking sources, but there are a variety of viewpoints on how concerned parents should be, how school districts can limit the amount of lead in water and what can be done if students are potentially impacted by elevated lead levels.
Megan Glover, CEO of 120WaterAudit, said in an interview with Education Dive last summer she finds it "interesting" that "there are no federal or state regulatory mandates for water testing in schools. I think we’re going to see that start to change."
Part of the problem has been a lack of education around the issue, Glover said.
"Many people aren’t aware that where the contamination happens is generally after the water leaves the treatment plant," she said, adding that students in post-industrial areas may be particularly susceptible, because of contaminants in the soil or piping. But schools and districts in rural areas, particularly those which are reliant on well water or "close to large agriculture, whether that be plants or animals," Glover said.
"But for the public water supplies, what we’re finding is that many school systems don’t know what the EPA regulations for water testing are," she added.
Another huge hurdle is cost.
"I think it goes back to budget and when could they realistically have budget to solve that problem and how does that problem rank in the priority list," said Glover. "Right now, from what I’m seeing, it’s falling as a school expense, a district expense, and the prices can vary depending on what you want to test for.
NYC and DC respond
Both the New York City Department of Education and the Washington, DC, system, which underwent its own system-wide analysis of water sources last year, say that there have been no cases of lead poisoning attributed to the drinking water in these facilities. A law signed in 2016 by New York Gov. Andrew Cuomo mandates that all schools statewide test for lead at the tap.
The NYC DOE noted the most potent source of lead exposure remained lead-based paint in homes. Kim Dietrich, Ph.D., a professor in the Department of Environmental Health at the University of Cincinnati who has studied lead’s effect on children for 40 years, concurred with that assessment.
“Children may be coming from older neighborhoods, where there is an older housing and where there is a significant amount more of a source than these water sources,” he said. “It is a much more significant source of lead exposure than in most communities, including Flint.”
Washington, DC, in particular, "does a wonderful job," Glover said. "They test every single tap that’s inside of the school level."
The Department of Urban Services has tested DC public schools for lead levels for years, but after Flint, the city decided to perform a system-wide analysis of all drinking sources, according to DC schools spokesperson Michelle Lerner. They used the EPA’s 15 ppb standard as a guideline.
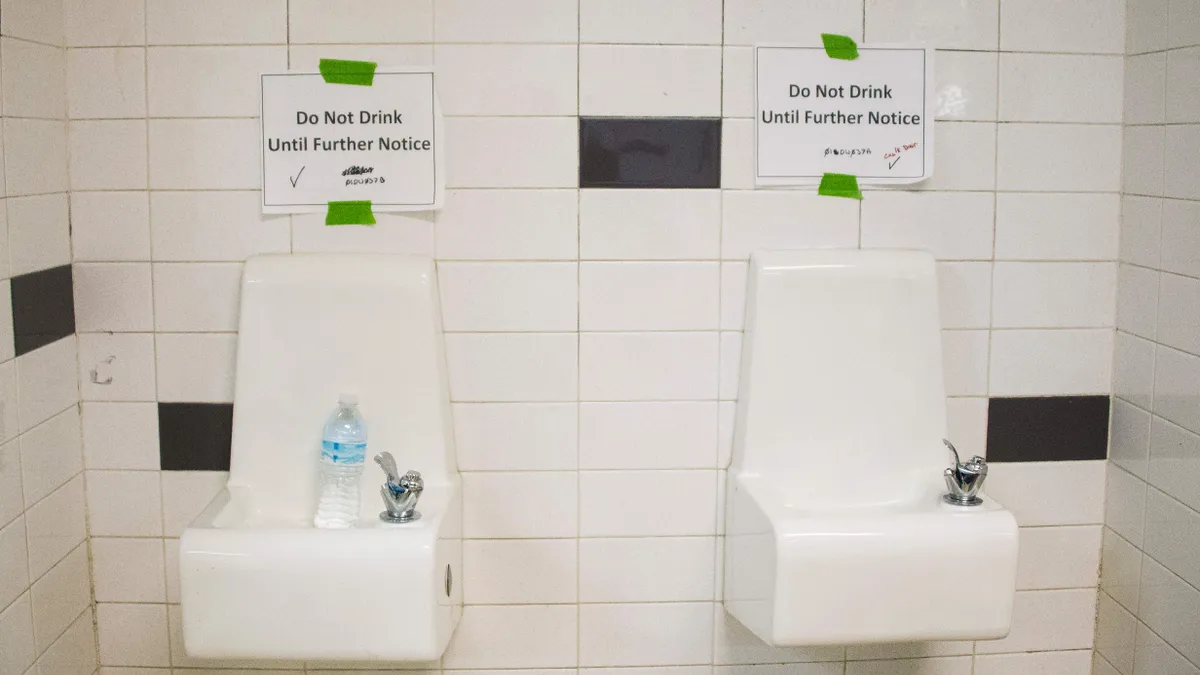
The city found 64 schools that had a water source test positive for lead levels higher than the standard, and DC responded by setting 1 ppb as its revised action level, far lower than the 15 ppb threshold. Lerner said the school system is in the process of ensuring that all drinking sources are filtered, and also fitted each non-drinking water source with picture warnings cautioning students not to drink from them. Officials also sent fact sheets to parents and communicated with families about the results of tests at their child’s schools. Lerner said a particular issue was that it could be difficult to discern the source of lead in a water source.
“It could be in the water, it could be in the pipes, it could be in the faucet,” she said. “If it’s in one place, it’s not necessarily coming from one source, it could be coming from a number of sources.”
In the case of New York, testing started in late November, according to a DOE spokesperson, with families receiving notice on a rolling basis. The testing included all charter schools inside of DOE buildings; city law also mandates that child care centers and Pre-K programs test their water for lead levels. The city said 8% of water sources tested registered levels above 15 ppb.
“We feel confident that the DOE is taking the right actions by taking drinking fixtures that have had lead exceedances off line until they can be replaced,” First Deputy Health Commissioner Dr. Oxiris Barbot said.
Expert maintains exposure can be mitigated by common treatments
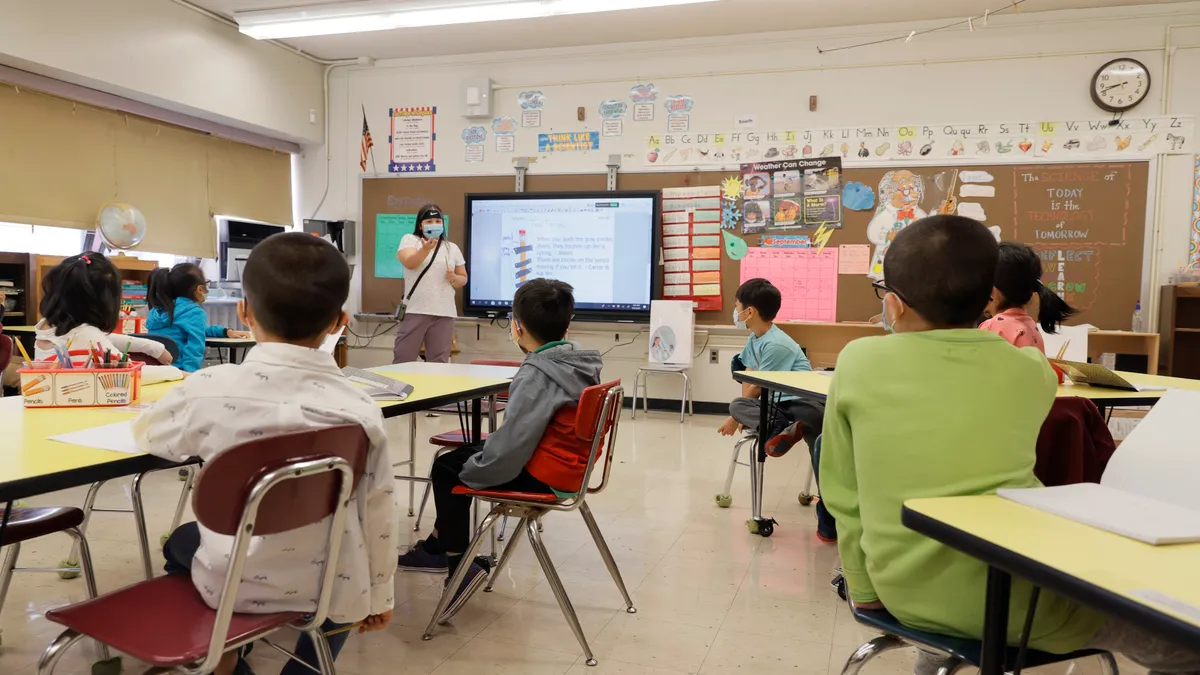
Acute lead poisoning is fairly rare, and can result in nausea, pain and muscle weakness, among a variety of symptoms. But chronic, low-level lead poisoning can occur over a longer period of time, and its impact may not be readily apparent to parents and educators. According to a 2015 report by the U.S. Centers for Disease Control titled “Educational Interventions for Children Affected by Lead,” neuropsychological performance could be impacted in a variety of ways, including deficiencies to “attention, executive functions, visual-spatial skills, social behavior, speech and language, and fine and gross motor skills.”
In the classroom, the results were equally distressing, with the report stating that studies showed a “strong relationship” between slightly elevated lead blood levels in younger students and lower end-of-grade test scores in elementary schools. The research indicated “a consistent link between low-level lead exposure and the reduced ability of children to do well in school and suggest that lead exposure is responsible for a significant and modifiable effect on the achievement gap,” according to the report.
"Especially in young, developing minds," Glover said, "any amount of lead exposure can lead to mental and physical" impacts which can be harmful to children.
Dietrich, who helped write the 2015 report, said that it could be difficult to discern how lower lead levels could factor into neurodevelopmental outcomes. Dietrich reiterated that the primary danger to children in terms of lead exposure came from older housing stock, particularly public housing built before 1978 when lead-based paint was outlawed.
But Glover said some infrastructure erected even later than that could be at risk.
"If the buildings were built even before 1986, there are chances that there are some lead components in the (infrastructure) whether that’s in the solder that’s used — it may not be the entire pipe — but 1986 was the cutoff for when they had to stop using any components of lead."
Dietrich said there could be potential long-term impacts for student performance and potential due to lead poisoning, and his research had indicated a correlation between elevated lead levels and exposure to the criminal justice system later in life, but he stressed how difficult it was to study long-term effects of lead exposure. Additionally, children in low-income communities are in particular danger of lead exposure, and this can make it difficult to measure direct impact, separate from the impact of other corrosive elements of poverty.
“Lead does not have a clear behavioral signature that we have been able to discern,” he said. “However, our work has shown that consistent elevations of blood-lead concentrations are associated with life-long deficits.”
“This is a trillion dollar decade problem, unfortunately, that were talking about in terms of infrastructure," Glover said. "The amount of investment in infrastructure since the 80s has been mostly flat, and any additional investment has been in repairing up the old infrastructure, just to keep it functioning."
But Dietrich decried the idea that the only way the issue could be solved in the immediate was an unimaginably vast refining of our nation’s infrastructure, including a complete revamping of water infrastructure in schools.
“I’m irritated by the fact that people say we have to spend billions of dollars to solve this — that’s not true. There’s a lot of things we can do in the interim,” he said, pointing to the importance of nutrition for impacted students, since lead absorbs in an empty stomach 50 to 100 times faster.
Generally, Dietrich found the conversation about responses to students potentially affected by lead exposure to be unnecessarily gloomy. He said the CDC’s research found that lead deficits were not immune to the treatments offered for a wide array of other learning deficits.
“The usual characterization of lead poisoning as permanent is totally and unduly pessimistic,” he said. “There’s no reason to believe that children who may have some deficits cannot be helped by the same programs utilized for children with learning problems and cognitive problems.”
He also stressed the need for more comprehensive testing of children in the country, pointing to a recent study which found that about 80% of children with elevated blood-lead levels in the country are not being adequately screened. He is worried that many children with higher levels have gone undiscovered. The concentration on specific regions or areas like Flint was important, but Dietrich worried it tended to obfuscate the more prevalent concerns that a wide array of lead exposure is not discovered.
“We seem to rediscover lead every three or four years,” he said. “And if you’re not screening children, you’re not going to discover the problem.”