Dive Brief:
-
As schools navigate another wave of COVID-19 related shutdowns, educators in rural areas are encountering resistance to precautions like masking and vaccination, sometimes exacerbated by conflicting or quickly changing guidance.
-
Rural areas have lower vaccination rates than urban centers, according to the Centers for Disease Control and Prevention. Although a sizable percentage of rural superintendents expressed interest in hosting COVID-19 vaccination clinics, 66% of the districts that said politicization of the pandemic posed a barrier are in rural areas.
-
While rural areas had lower COVID-19 transmission rates at the start of the pandemic than more heavily populated urban areas, those same areas are tackling severe staff and substitute shortages as positive test rates have grown.
Dive Insight:
“In the beginning of all of this, the one advantage the rural communities had was they were more isolated,” said David Little, executive director of the Rural Schools Association of New York State. “And it almost led, in the initial stages, to [an attitude of] ‘this really isn't about us.’”
But as the omicron variant spreads, rural schools are struggling to stay open just like their urban and suburban counterparts are.
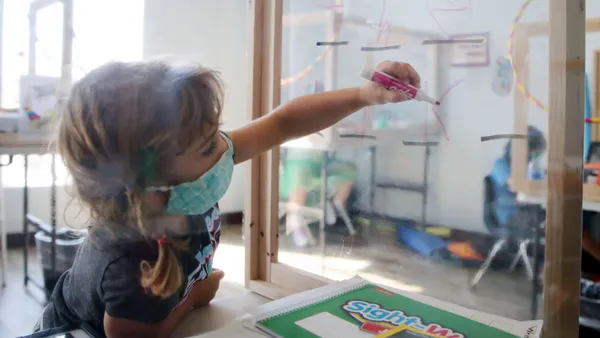
Parents and students have adhered to safety measures like social distancing, handwashing and sanitizing in school buildings for the most part, according to both Little and Kristi Windsor, deputy director of Monroe County Schools in Tennessee.
The adherence comes as a result of a “tremendous desire to keep the school going,” said Little.
Windsor has seen more resistance toward mask and vaccine mandates, adding that in rural communities like hers, “it tends to be that people are less accepting” of those requirements.
Janet Farmer, district head nurse in Wyoming’s Laramie County School District 1, which serves rural areas, said community response and resistance to precautions like quarantines and isolations have made nurses’ jobs more challenging, especially this year. “I've had nurses get yelled at, get hung up on and get cussed at,” Farmer, whose district includes 34 schools serving 13,000 students, said.
“We’re usually the good guy,” she said. “This year, we are the bad guy.” Farmer said out of the nurses she oversees, she expects a handful to quit as a result.
Resistance has been made worse by quickly changing, and sometimes conflicting, guidance from local and federal authorities around COVID-19 health precautions and requirements.
“It makes your job very difficult,” said Windsor, who has been accused by some in the community of withholding, changing and not correctly adhering to COVID-19 safety recommendations.
Likewise, Linda Mendonca, president of the National Association of School Nurses, said changing guidance and requirements fracture trust between nursing staff and the communities they serve.
In the meantime, test-to-stay has become a popular option for maintaining in-person learning, Little said. However, testing isn’t as easily accessible in rural areas as in large urban or suburban settings.
Calling it “impractical,” Little said, “Most people in urban and suburban areas go to Walgreens or CVS, and/or there's a state testing site. Those don't exist in many rural areas.”
Farmer’s schools, for example, had to forgo a test-to-stay program because it wasn’t logistically feasible to get a large number of tests or have the staff to administer them. Those looking to test outside of a school setting do so at local urgent care, which can have lines up to three hours long, Farmer said
In other areas, staff in rural schools — with resources and personnel already stretched thin — often become test providers and contact tracers. Combined with more individuals testing positive, a preexisting substitute teacher shortage, and limited staff to organize COVID-19 vaccine clinics, schools could shut down at the drop of a hat.
“If it's bad everywhere, it's really bad in rural areas,” said Little. “Rural schools are provided the least amount of resources.”