Do your school staff members have gatherings or activities to help them build relationships with each other?
Is there a process for collaborating with community-based behavioral health providers for students who need support?
Does your district track schools’ use of social-emotional learning, trauma-informed practices or other efforts to support students’ and staff members’ well-being?
Those are among the questions school and district leaders can ask themselves as part of a growing initiative to respond to the adverse childhood experiences — or ACEs — research has shown can impact school performance and long-term health outcomes.
Called Resilience in School Environments, the effort is part of the Thriving Schools program at Kaiser Permanente, which 20 years ago took part in the landmark study on the issue with the Centers for Disease Control and Prevention. Almost two-thirds of participants in the study reported at least one experience of abuse, neglect or household dysfunction before age 18, and more than one in five reported three or more ACEs.
Through a partnership announced Thursday with nonprofit Alliance for a Healthier Education and Discovery Education, the RISE program will bring on-site and virtual resources to schools focused on the social and emotional health of both students and school staff members, with plans to reach 25,000 schools by 2023.
"The additional resources will help our staff manage through stressful situations and reinforce the power of a well-established support system for our colleagues and the students in our classrooms," says Rachel Sherwood, principal of Bemiss Elementary in the Spokane Public Schools, one of 633 schools and 36 school districts participating in the program.
The centerpiece of the program is the RISE index, an assessment tool schools and districts can use to ask questions about school climate and the conditions that can support students’ and staff members’ mental wellness. There is an index for schools as well as for districts, which asks, for example, if there is a district-level leadership team focusing on social-emotional health.
'A facilitator or a barrier'
Thriving Schools, which began in 2013, originally focused on healthy eating and physical exercise — and the program saw results, such as increases in the amount of physical education for students, says Annie Reed, director of the program.
But she suggests the focus on physical health didn’t go far enough.
“With resilience, there is such a direct connection to what [teachers] see in the classroom,” she says. “The issue of social-emotional health can be a facilitator or a barrier to what they’re trying to accomplish.”
A “landscape analysis” also showed while there were a variety of approaches focusing on the trauma students may have experienced, schools lacked similar programs for educators.
“What are the systems that teachers need so that they can regulate?” Reed asks. “Does the school have a policy that allows teachers to take a break?”
Meanwhile, Blue Shield of California, another health plan provider, has launched BlueSky, a student mental health and teacher training initiative beginning in the Oakland, San Leandro, Sweetwater Union and Oceanside school districts.
Roughly 20,000 students in 19 middle and high schools will have access to mental health clinicians from nonprofit Wellness Together, and the National Alliance on Mental Health California will help students form peer groups in schools to reduce the stigma around mental health issues. Online resources related to promoting positive mental health will also be available on DoSomething.org.
"Educators are on the front lines in recognizing adverse childhood experiences as a public health crisis,” California’s Surgeon General Dr. Nadine Burke Harris, said in a press release about the initiative. “This collaboration is truly about the intersection of education and health."
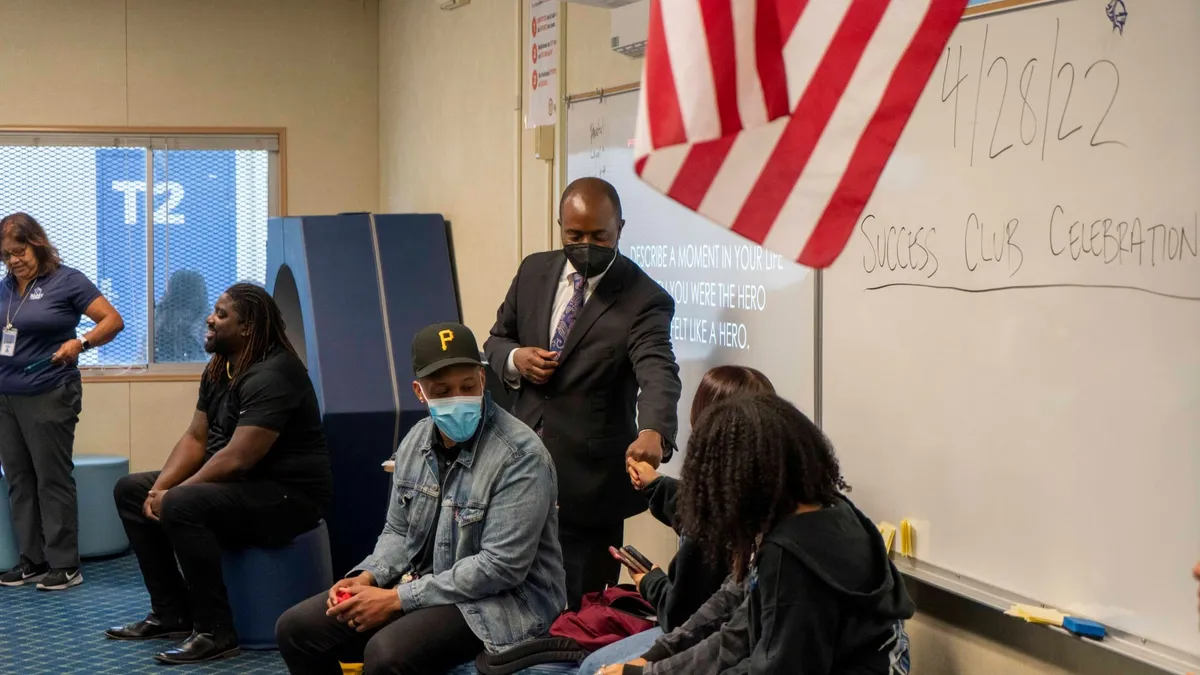
At, Coliseum College Preparatory Academy, a grades 6-12 community school in the Oakland Unified School District, the school’s health clinic conducts scans among students. Figures show roughly 40% of the students per grade have experienced trauma, says Principal Amy Carozza. Rosalind Kingsley-Hurst, a consultant from Wellness Together, is now working with staff members to organize groups for students facing similar issues.
“We can have lots of great ideas, but you need to have the people to do that work otherwise you’re taking kids out of the learning space and into nothing,” Carozza says. “Over seven years you really have to take a long view of what kids need and appropriate mental health support becomes a reasonable strategy when you’re looking at a seven-year commitment to kids and families.”
The role of schools in screening for ACEs
Along with the state’s Department of Health Care Services, Burke Harris last week launched ACEs Aware, an effort to train primary health care providers participating in the state’s Medicaid program to screen children for ACEs. Beginning in January, providers will be able to bill Medi-Cal for the screenings if they use a particular tool developed at the University of California San Francisco.
Burke Harris has been outspoken about screening for ACEs in children before they reach school, but in an interview, she says her statements have been misinterpreted and she wanted to clarify her position on the role of schools in the screening process.
"The place for the screening is in the doctor's office," she says, adding that having healthcare providers conduct those assessments is important for maintaining "public confidence" in the process. "Educators have more than enough to do. I feel like there is an even more important role tor educators to play than screening."
That role, she adds, is giving students "daily doses of interaction" that can help them develop skills to "regulate themselves."
The research on resilience shows at least one stable, caring relationship with a parent or caregiver, a sense of self-efficacy and skills to cope with stress are among factors that can “stack the scale” with positive influences for a child who has experienced significant hardship.
Burke Harris, however, did suggest school districts should begin requiring students to be screened for ACEs, in the same way they are required to show proof of immunization. She adds, however, a student's ACEs score — the number of adverse experiences in a child's background — should not be shared.
"We know that ACEs profoundly impact a child's ability to learn," she says. "If educational leaders recognize and respond to that," children have better opportunities to succeed.
Ongoing research
These efforts also come as researchers are learning more about the links between ACEs and leading causes of death, such as heart disease. Drawing from a sample of 144,000 adults across 25 states, a November study from the CDC showed 61% of adults had at least one ACE, and 16% had four or more types of early adverse experiences.
Preventing those experiences, the authors write, could have reduced the number of adults with heart disease by up to 13%, the number with obesity by 2% and the number with depression by 44%. “Improving school environments to lessen the impact of ACEs and prevent further trauma” is one of the strategies highlighted in the findings.
In addition to expanding its Thriving Schools program with RISE, Kaiser is also spending $2.75 million to fund new research into which protective factors can prevent ACEs, how to lessen the impact of trauma throughout one’s lifetime, and which community-based services can address ACEs.
Christopher Blodgett, a Washington State University Extension clinical psychologist and researcher who has conducted ACEs screenings as part of research studies in Head Start and in Spokane elementary schools, says while “a lot of kids are doing just fine,” the effects of segregation by income and ethnicity in the U.S. have resulted in schools where there are “deep concentrations of these problems.”
He also thinks screening for ACEs in a school setting is inappropriate.
Screenings, he says, make sense in a healthcare environment, but the education sector does not have “an equivalent structure.” A routine screening process might identify which students have experienced trauma, he says, but schools can often “do zip about it.”
Burke Harris agreed screenings lead to questions about how schools can adequately respond. That's where programs like RISE and BlueSky come in, she says. She also noted the work of the Center for Wellness and Achievement in Education in San Francisco and Turnaround for Children in New York City as examples of successful models of addressing trauma and adversity in children.
Blodgett adds there are also privacy concerns when schools conduct ACEs screenings. “Have you thought through how you are going to protect this data?” he asks. “You’re asking for sensitive information.”
A 2016 guide from the National Center for Mental Health and Juvenile Justice and the Defending Childhood State Policy Initiative says screening can be “a useful tool to determine potential risk for stress or trauma among students in schools.”
But the authors also noted several concerns, including the potential for stigmatizing students. Also, simply discovering whether students have experienced one or more traumatic events doesn’t mean they will struggle throughout their lives or develop serious health problems.
Only a minority of those who have experienced trauma “will ever demonstrate clinical symptoms of traumatic stress,” the guide says. “Even a known stressor leading to a known traumatic response does not perfectly predict negative school or life outcomes.”
Blodgett adds while he understands the sense of urgency among educators, there’s not enough research on ACEs screening in a school setting. “We need to own the fact that we don’t know right now,” he says.
Rather than implementing universal screening, he says in most schools, teachers already know which students need more targeted mental health support. “Our experience suggests that you can do this in a fairly safe way by using the knowledge you already have,” he says.
“Have you thought through how you are going to protect this data?”

Christopher Blodgett
Clinical psychologist and researcher, Washington State University Extension
A systemic approach
WSU Extension’s Child and Family Research Unit, which Blodgett directs, also runs a professional development and consultation program in schools — Collaborative Learning for Educational Achievement and Resilience — to help educators better understand trauma and how to intervene. Over a period of three to four years, CLEAR consultants, become “part of a problem-solving team,” Blodgett says. Since 2013, CLEAR has worked with schools in five states.
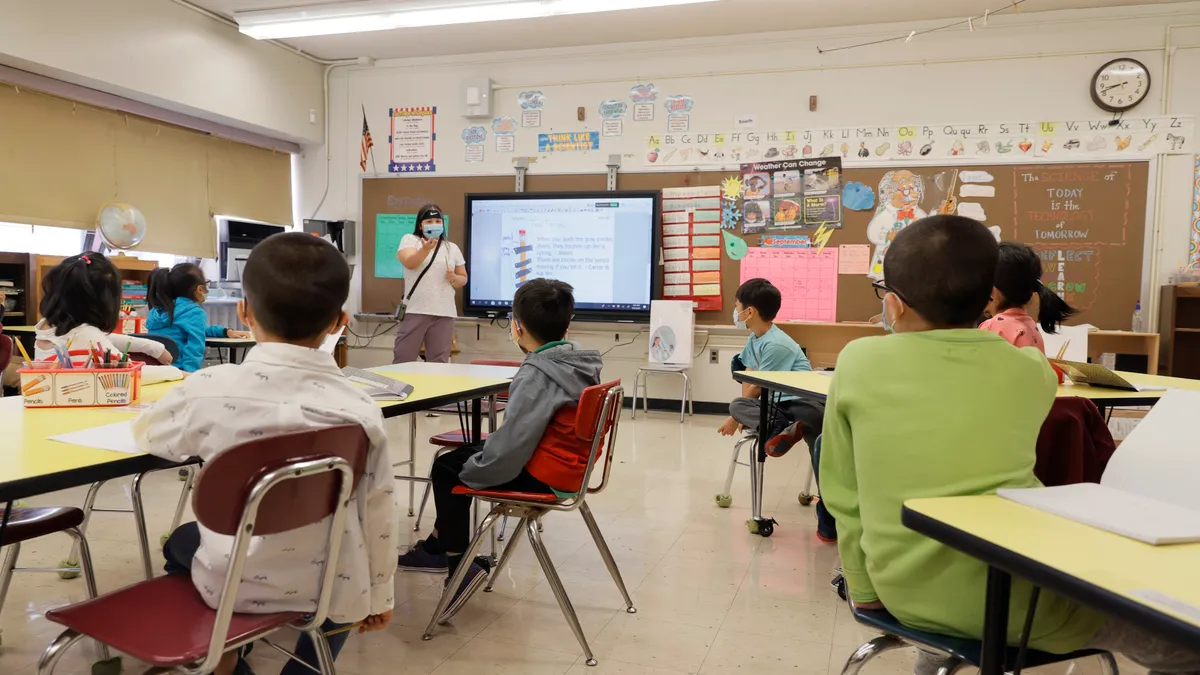
Eisenhower Elementary in the Vancouver Public Schools in Washington became part of CLEAR after finding roughly one in four students had experienced past or recent adversity, and because trauma-informed practices was one of the teachers’ most-requested topics for professional development, says Principal Jennifer Blechschmidt.
Blechschmidt says she sees two distinct areas of need among students — “externalizers” who show aggressive behavior such as assault, property damage and/or self-harm, and “internalizers” who become isolated, have poor attendance and struggle to have friends. Both groups, she says, face challenges academically.
The CLEAR consultant works on a monthly basis with the staff to provide professional development and consultation regarding specific students. Blechschmidt says it’s important to have a professional who not only understands students’ needs, but also “understands the needs of teachers who continue to support those students on a daily basis.”
Changes in the classroom have included adding “safe spaces” for students, holding community circles, using specific strategies focusing on self-regulation and “using hand signals that demonstrate connections between calm brains and ‘flipped lids’ that is easy for all students to understand and access,” Blechschmidt says.
RISE, Blodgett says, also has the potential to “reshape the conversation around trauma in schools.” But screening students won’t be part of the program.
Reed says the healthcare provider is taking a “population health approach” by focusing on policies and how schools are structured to support students’ well-being.
“They’re embracing that this is a systems problem,” Blodgett says, “and it’s going to require systems solutions.”