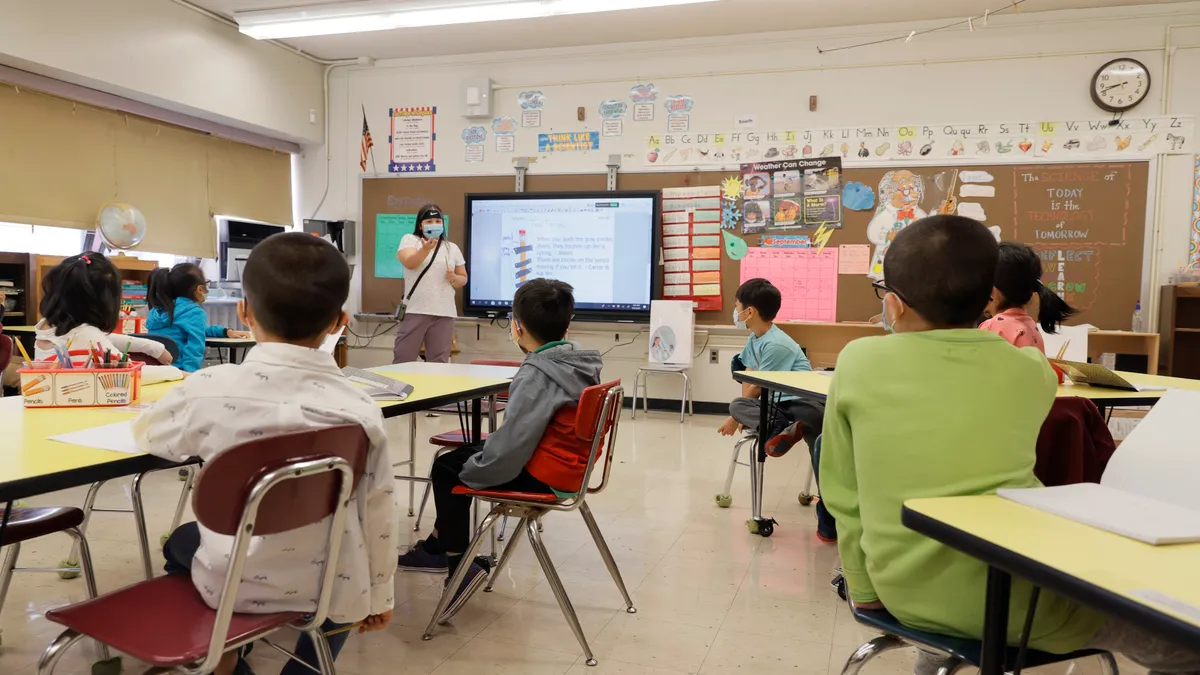
In nearly three decades as a school nurse, National Association of School Nurses President Laurie Combe has dealt with her share of infectious diseases.
Before COVID-19, there was measles, tuberculosis and swine flu, which all required similar precautions, such as quarantine, contact tracing and educating the public about the risks of exposure and the benefits of immunizing children for prevention.
“The reason we immunize children is because not only can they spread disease within the school community where it would have so much contact; but if we protect them in the school, we’re also protecting the broader community from the spread of these preventable diseases,” she said. “So the school really has a huge role to play in the health of the broader community.”
Yet so much of what that will look like remains unclear, even with the recent news of COVID-19 vaccines trials’ promising results.
Meanwhile, amid a nationwide school nurse shortage in a country increasingly divided over the coronavirus and school reopening plans — not to mention declining support for regular immunization requirements for children — some education advocates worry whether schools will be ready to help when the time comes.
Challenges ahead
Dr. Mario Ramirez, managing director of Opportunity Labs and a senior fellow at FutureEd in the Georgetown University McCourt School of Public Policy, said schools have played “very active” roles in vaccinations in prior epidemics. “I think given the breadth and the scope of this pandemic, it’s certainly reasonable to feel like schools could play a role there — a very valuable role,” he said. “They touch so many more people than any other public institution.”
Yet Ramirez, a physician and former acting director for the federal Office of Pandemic and Emerging Threats, said schools face two major hurdles: logistics and public trust.
A quarter of schools in the U.S. have no school nurse, and others may have someone part-time who splits their hours between several schools, according to NASN research. Fewer than 40% of schools have a full-time employee.
Additionally, a survey of NASN members from earlier this year shows many felt their schools weren’t ready for a COVID-19 outbreak.
Storing a COVID-19 vaccine in schools could also prove difficult, Ramirez said.
“There are several vaccine candidates. The Pfizer vaccine has to be stored at temperatures that are so cold that schools wouldn’t really be a valid distribution point unless there were movement of ultra-cold freezers out to schools, which I don’t think anyone sees as possible,” he said.
Preliminary data from Pfizer trials show its vaccine to be 90% effective in study participants. The company expects to produce up to 50 million doses of the vaccine this year and up to 1.3 billion in 2021, according to a Nov. 11 news release.
Johnson & Johnson, AstraZeneca and Moderna are also among companies with vaccines on the way in coming months. But Moderna Chief Medical Officer Dr. Tal Zaks has warned that a vaccine still may not stop the spread of the virus — a detail likely to further complicate the issue.
Guidance from the National Academies of Science Engineering and Medicine also suggests COVID-19 vaccine availability to children may still be a long way off, however, and Ramirez doesn’t see that happening this school year. Healthcare workers, older adults and those with comorbid conditions are among the first groups that will have access to a vaccine in the first of four phases. K-12 teachers and school staff are included in phase two, and children will be part of phase three, according to NASEM.
“There are some logistical concerns that are going to need to be ironed out over the next two to three months, but then all of that is wrapped into the bigger societal issues, as well,” said Ramirez, who co-authored a recent opinion article for The Hill asserting public schools aren’t ready for the “long-simmering national debate over childhood vaccination” that’s barrelling toward them.
In 2015 and 2019, 84% of Americans believed parents vaccinating their children was very or extremely important, down from 94% in 2001, according to Gallup.
“As far as it relates to COVID-19, six months ago, public interest in vaccines/vaccination was really high, and then all the political infighting tied to the presidential campaign and concerns about the safety profiles, many of which were just kind of rooted in conjecture, drove down confidence in the [vaccine],” Ramirez said.
Combe said some people are also hesitant because of the speed of the federal government’s vaccine development process, dubbed Operation Warp Speed.
Gallup data from September shows only 50% of people surveyed have said they will get the vaccine, down from 61% in August and 66% in July. But, Ramirez said: “I expect those numbers will shift some as we get actual reporting about the side effects profile and how efficient it is."
Schools at work
Combe said states are in the planning stages of what a vaccine rollout will look like, and NASN does not have data on what would be required of schools. Yet she knows some school districts are at work building community trust in preparation for a vaccine.
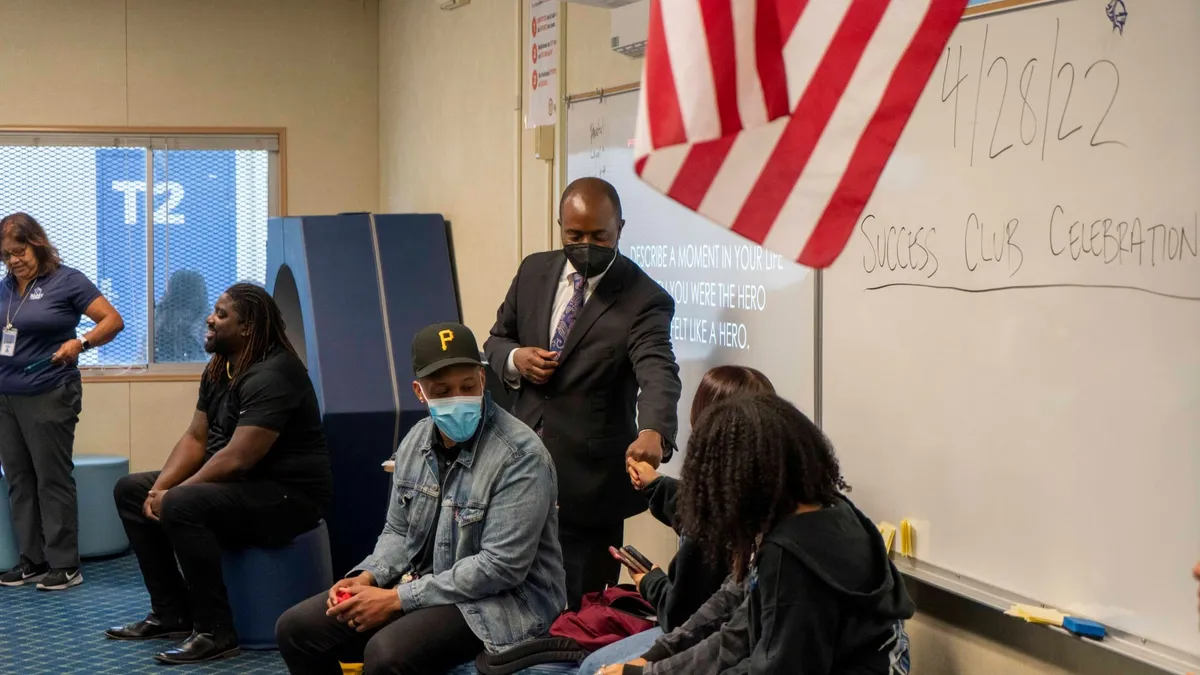
In South Carolina, for example, the Charleston County School District added to its school nursing staff of more than 100 this school year, ensuring at least one full-time nurse at each school. The district also added an immunization coordinator position, said Director of Nursing Services Ellen Nitz.
While these changes have more to do with a federal Vaccines for Children grant the school received, in order to offer required immunizations at no cost to children who cannot afford them through a healthcare provider, Nitz said COVID-19 tipped the scale on the district’s decision to boost its nursing numbers.
“I think that school nurses are going to be important when we get the COVID-19 vaccine,” she said. “I think it’s going to be all hands on deck for all of our healthcare providers ... but also healthcare providers such as my school nurses, that we would step into the public health role and be able to assist by providing those vaccines to those that need them.”
Nitz said South Carolina has surveyed schools asking if they would be willing to help when a vaccine is available, though it’s not yet clear how.
“People normally feel that school is a safe place,” she said. “If we were asked to be able to host vaccine clinics in a school setting, that already kind of makes people feel a little bit more at ease versus having to go through a health department that they’re not as familiar with. So, anytime you can help to decrease people’s anxiety, I think that’s always going to be in your favor.”
In New Mexico’s Alamogordo Public Schools, school officials are also working to build trust with the local community a renovated 20-year-old Winnebago RV named “Flo,” after one of history’s most famous nurses, Florence Nightingale. The district has used the mobile unit for COVID-19 and antibody testing, as well as other community outreach, and it plans to do vision and hearing screenings for children as it would during a normal school year.
“When [a vaccine] does come, we’ll have means to disburse that appropriately,” said Alamogordo Superintendent Jerrett Perry. “We’re going to do whatever it takes.”